Inspired by nature: the thrilling new science that could transform medicine | Laura Parker

The Long Read: Jeffrey Karp is at the forefront of a new generation of scientists using natures blueprints to create breakthrough medical technologies. Can bioinspiration help to solve some of humanitys most urgent problems?

In the summer of 2005, Jeffrey Karp, a bioengineer at Brigham and Womens Hospital (BWH) in Cambridge, Massachusetts, was working late one night when he spotted a journal article on a colleagues desk. What caught his eye was not the text itself, but the full-page colour illustration of Spider-Man that accompanied it. Intrigued, Karp sat down and started reading.
The article detailed how a group of researchers had created a new synthetic material by mimicking the properties of gecko feet whose tiny, hair-like pillars allow the lizard to stick to and detach from apparently sheer surfaces with ease. Imagined uses for the material included gloves that would allow military personnel to climb up the sides of buildings, just like Spider-Man.
The wheels in my head started turning, Karp told me recently. His first thought was to use the material to create a new type of medical tape that could replace sutures and staples, which can damage sensitive tissue surrounding wounds. Karp was working alongside the world-renowned bioengineer Robert Langer at the time, studying ways to create biodegradable materials that could seal wounds inside the human body. The tape could even go a step further than sutures or surgical staples, he thought, and be used in particularly intricate surgical procedures for instance, tying together the small intestine during gastric bypass surgery.
The next morning, Karp stopped by Langers office and convinced him that he had come up with the perfect idea to win a prestigious research grant. But as he began his research, Karp found that it wasnt enough to simply rely on friction between the hair-like pillars to make the tape stick. That may be how geckos feet work, but he was going to need something much stronger if he hoped to bind human tissue inside the body.
When he tried coating the surface of the tape with a glue, Karp found that it seeped in between the pillars, like honey drizzled on to a hair brush. Next, he played around with the position of the pillars on the surface of the tape, placing them closer together. That didnt work either when the pillars were too close together, there wasnt enough friction with the surface of the tissue. So he moved them apart again, and then tried coating each individual pillar with the glue, instead of simply brushing it over the top. Now, whenever the tissue came into contact with a pillar, it stuck in place. Finally, Karp had his solution.
It was a great example of a holistic approach to problem-solving, David Kaplan, chair of the biomedical engineering department at Tufts University in Massachusetts, told me. In 2008, MITs Technology Review magazine named Karp one of the top innovators in the world under the age of 35.
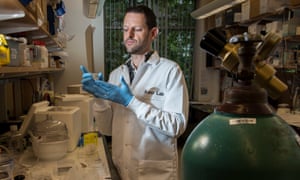
Karp, who is now 40 and runs his own lab at BWH, is what is known in the business as a bioinspirationalist a person who looks to nature for solutions to scientific problems. The gecko tape was Karps first bioinspired invention; these days he is regarded as a leading figure in the field. (He often tells people that he owes his success to Spider-Man theres a large drawing of the Marvel superhero in his office, and he once wore a Spider-Man T-shirt during a TEDMed talk.) Karps current projects include surgical staples inspired by porcupine quills, which create smaller punctures in the skin and prevent bacteria from entering wounds, and a new kind of surgical glue inspired by the sticky secretions of marine worms, which is strong enough to bind moving tissue inside major organs, such as the heart.
This last invention has helped to cement Karps reputation as a rising star in the world of bioengineering. Because he doesnt just invent cool stuff he turns his creations into actual products. When we look to solve problems, its not so we can publish papers and get pats on the back from the academic community, said Nick Sherman, a research technician at Karp Lab. Its more like, Is this work going to help patients? If not, how do we make it help them?
Earlier this year, Karps surgical glue began a human clinical trial in Paris. It is the first of Karps innovations to advance this far. Unlike other surgical glues on the market, his actively repels blood, making it ideal for sealing holes in blood vessels, intestinal tissue, even bone. It is also much sturdier, meaning that surgeons could use it to fix cardiac defects without the need for open heart surgery. This could completely transform how we perform surgery, said Jean-Marc Alsac, the cardiovascular surgeon at the Hospital European Georges-Pompidou in Paris who is overseeing the trial.
Karp Lab, which opened in July 2007, is hidden behind a heavy white door on the third floor of an office building in Cambridge, near Massachusetts Institute of Technology. Inside, a stockpile of white lab coats hangs near the entrance, and beyond lies a jigsaw puzzle of heavy machinery, vials, tubes and jars, sanitising stations and discarded rubber gloves. Lots of labs are doing what appears to be similar work but, truly, they are not in [Karps] league, Arnold Caplan, a professor in the department of biology at Case Western Reserve University in Cleveland, Ohio, told me.
Every Wednesday at 8am, staff meet in a large conference room to discuss ideas. The lab employs around 25 staff, from undergraduates to postdoctoral fellows, although its ethos is strictly non-hierarchical. One research trainee, Thomas Kuncewicz, joined Karp Lab just over a year ago, before finishing his undergraduate degree, and is now leading two projects. Everyones experience is different and thats what matters most here, he told me. Not some dumb pyramid scheme where we have to work our way up through the ranks. Lab employees are encouraged to email Karp whenever they have a question or idea. If you ever email him, within five minutes youll have a response, Kuncewicz said. It can be 11pm or 3am, and hell reply. (I have exchanged emails with Karp long past midnight. His average response time is about 10 minutes.)
The lab attracts the kind of budding scientist who wont turn up their nose at the occasional lab outing to the zoo or the aquarium. A couple of years ago, one of Karps students returned from a field trip with a handful of porcupine quills. At the time, Karp was in the middle of designing a new type of surgical staple, which are most often used in surgery to close sensitive wounds that cannot be sutured by hand. Karp looked closely at the quills and noticed that each had multiple tiny barbs on the end of its tip, like a serrated knife. He took a few quills and stuck them in his chin to test how much force would be required to puncture the skin, and how much it would hurt. (Surprisingly little, he said later.)
Over the next few months, Karp designed a surgical staple with serrated ends, like the quills. He tested it on raw chicken and found it slid in easily, and created small, clean holes that caused virtually no damage to the surrounding tissue. The staples that are currently in use cause large punctures in surrounding tissue which allow more bacteria to enter the wound and cause infection. Karp Lab patented the staple and is working on getting it to market. Karp believes that the invention could significantly reduce post-surgery complications, which are often caused by current surgical staples.
For Karp and others in his field, nature often holds the key to critical scientific and medical problems. This approach also gives scientists free access to a vast number of solutions that have already benefitted from millions of years of trial-and-error testing. The appeal of bioinspiration, for Karp, lies in the idea that every living creature that exists today is here because it tackled a number of challenges. And those that havent have quickly become extinct, he said. In essence, we are surrounded by solutions. Evolution is truly the best problem-solver.
A distinct advantage of the bioinspiration route is that pre-existing solutions are somewhat handed to us, Leif Ristroph, an assistant professor of mathematics at New York Universitys Courant Institute, told me. Of course we have to figure out the mechanisms behind the solution, and determine which parts we care to mimic and which do not carry over to our problem of interest. The leaf as natures solar panel is a great example: scientists have been trying to better understand photosynthesis for a long time, even well before we wanted to collect and store solar energy ourselves.
In recent decades, advances in technology, engineering, and robotics have made it easier to observe nature and borrow from it with more precision than ever before. In the early 2000s, Japan Railways Group, which operates the Shinkansen bullet train, asked one of its engineers, Eiji Nakatsu, to come up with a way to fix a longstanding problem. Whenever the train went through a narrow tunnel at high speed, the atmospheric pressure created low-frequency waves that spread out from the tunnel and created vibrations in the air. These vibrations were so powerful that residents 400 metres away from the railway line wrote in to complain about the noise.

Nakatsu, who is a keen birdwatcher, wondered if his weekend hobby might provide him with ideas for how to deal with sudden changes in air resistance. His mind turned to the kingfisher, a bird whose long and flat beak allows it to dive from the air (low resistance) into water (high resistance), with a minimal amount of disturbance so as not to alert its prey. Nakatsu redesigned the nose of the Shinkansen 500-Series, making it longer and flatter. The new design successfully reduced air pressure by 30%.
The story of Nakatsu and the Shinkansen is a favourite among advocates of bioinspiration. Many of the worlds top academic institutions Harvard, Oxford, Stanford, and Columbia now offer courses in bioinspired engineering, while organisations such as the World Biomimetic Foundation and the Biomimicry Institute have been established specifically to help spread the word by highlighting the work of companies who dabble in bioinspired design an electricity-free ventilation system modelled on termite mounds, for instance, or wind turbines with aerodynamic bumps similar to those found on a humpback whales flippers.
Still, even those who believe that bioinspiration may hold the key to solving humanitys most urgent problems water scarcity, overpopulation, climate change are careful to point out that the field is still in its infancy. Beth Rattner, the executive director of the Biomimicry Institute, told me: We can observe and make mathematical replications of a kingfisher beak on the nose of a train, but were still unable to fully emulate or replicate a lot of biological phenomena, either at all or to the point where its commercially viable.
Biomimicry should be considered as a means to understand nature and conceive engineering design, but not as a dogma, says Maurizio Porfiri, a professor at New York Universitys Tandon School of Engineering. In other words, while evolution has pursued an optimal path from swimming to flight this happened in a specific context, with specific constraints. Even Leif Ristroph concedes that he would not, for example, slavishly copy a bird or insect in order to design a robot. Clearly, birds inspired the basic design of aeroplanes, but the early designs with flapping wings did not win out, he said.
Still, Karp is not suggesting that scientists copy nature directly. Instead, he wants to look at what works and improve on it. The key is to analyse the solution evolution has converged on, and then take advantage of those principles in an engineering context, Adrian Thomas, professor of biomechanics in the zoology department at Oxford University told me. The obvious mistake is to copy nature it is possible to do much better than nature by exploiting the best engineering materials.
While research labs dedicated entirely to bioinspiration are rare, Karps is not the only one. Don Ingbers Wyss Institute at Harvard University, which has been running since 2009, is a bioinspiration factory. There are some 375 full-time staff, who together enjoy more than $600m in grants and philanthropic funding. The lab has co-founded 15 startups in the last three years, and has more than 15,000 patents out for a range of bioinspired technology and designs across a range of disciplines, from medicine to robotics. They include a self-organising swarm of tiny robots that can be used for tasks such as surveillance, traffic monitoring and crop pollination, and a mattress that senses the cardio-respiratory functions of infants and can help detect when they are having trouble breathing. Jeff has done amazing stuff in his lab, Ingber told me. But we can do it much faster. Were able to take much bigger risks here, and were more likely to succeed, both technically and commercially.
But sheer volume is not Karps aim. When the lab first opened, Karp thought he might use bioinspiration to tackle problems around cell migration, the process whereby cells move around an organism to aid in tissue formation, wound healing and immune response. That same year, after speaking at a biomedical conference to drum up support for the lab, someone approached Karp and told him bluntly that the only interesting thing about his talk was the gecko tape. Thats all people asked me about, Karp told me. So that got me thinking, maybe I should just focus on medical devices. It seemed to be the thing that got people excited.

One evening in August 2009, Karp received an email from Pedro J del Nido, a specialist in cardiac surgery at Boston Childrens Hospital. Del Nido was having difficulty sealing holes in the hearts of young patients suffering from congenital heart defects. Whenever Del Nido tried to suture a hole, the surrounding tissue would tear. He had read Karps paper on the gecko tape, and wondered if Karp could help him design something similar to help treat his young patients.
This presented a new challenge for Karp. While the gecko tape can seal things like tissue and gastrointestinal tracts, the heart is not stationary. It moves very fast and violently, as blood constantly gushes in and out. Any adhesive would have to be strong enough to resist being washed away in the deluge. Karp wondered if a surgical glue might help solve Del Nidos problem. Gluing internal surgical wounds is quicker and sometimes more effective than stitches, particularly around sensitive areas where any rip or tear in the skin will damage surrounding tissue. But Karp did not know any surgical glues that could work successfully in the presence of a lot of blood, and none that are strong enough to actually bind moving tissue. Whats more, surgical glues sometimes have harmful side-effects (such as releasing formaldehyde inside the body) and can take as long as 30 minutes to set. As any surgeon will attest, the less time a patient lies on the operating table with their insides exposed, the better.
Karp told Del Nido that he would try to come up with something. Except, he didnt really know how. The gecko tape had been an academic invention. There had been one animal trial on mice. Del Nido needed something practical that he and his surgeons could actually use when operating on children. Karp realised that if he was going to help Del Nido, he had to talk to some people who had experience turning inventions into products. One of the reasons most medical devices invented in an academic environment never make it to patients is because theyre so complex and you cant manufacture them at the right scale, or at the right price, Karp told me. The lab is really just the first step.
Karp decided that he would need to build his own network of contacts: entrepreneurs, venture capitalists, patent attorneys, regulatory body contacts, consultants, and business managers, who would be familiar with his methods and guide him on every step of the process. He spent the next two years meeting with venture capitalists around Boston, attending networking events sponsored by local law firms, consulates and biotech companies. He flew around the country presenting his work to various companies. I wanted to make it in such a way that as soon I came up with an idea, all Id have to do is just fire off an email to the right person and that would be it, he said.
One morning in late June, I accompanied Karp on a visit to the New England Aquarium in Boston. Scientists have a reputation for being slightly awkward, but Karp is at ease in his own skin. Tall, with a lean build and slight stubble, he peppers lengthy scientific explanations with jokes, usually at his own expense. Stop me if I get too boring, is something he says often. He is fond of drawing diagrams to explain what he is talking about. Hes one of those very rare scientists who can talk to everyone at their level, Sherman, the Karp Lab research technician, told me. How he talks to high-schoolers is different from how he talks to PhD fellows, and thats different to how he talks to physicians. But its always at the same level of excitement.
Karp grew up in Peterborough, a rural county in Ontario in a Frank Gehry-designed house that his parents bought from a local builder. The family moved in when Karp was eight; it was his first time living outside the city. There was a buffalo farm across the road, and a sheep farm next door. There was a creek running through the backyard, and the property backed on to a forest. I would wake in the middle of the night, said Karp, and there would be a pack of wolves on my front lawn headed to the sheep farm for a snack!
Karp began taking trips into the woods, looking for snakes. Later, he would mount expeditions to trap frogs and snapping turtles by the creek. He got used to seeing foxes on the driveway at dusk and listened out for the hoots of the great grey owls nesting nearby. For a kid with no appreciation of nature, this was a really big turning point for me, he said. It was like, here was this whole new world I never even knew existed.
Inside the aquarium, Karp led me to a large, fluorescent tank filled with lions mane jellyfish, one of the largest species, with a bell-shaped hood that can reach eight feet in diameter and tentacles that can stretch over 100 feet. The key thing to remember is that the problem comes first, not the solution, Karp said, peering inside the tank. We dont sit in front of the jellyfish tank and think, How can we design a medical device that does what these jellyfish do? Its more like, we have a problem we need to solve, and these floating piles of jelly might be able to help us.
A few years ago, Karp began looking at jellyfish to try and improve the design of a blood analysis device that can detect whether a cancer has metastasised after the removal of a tumour. Devices like this already exist: they resemble a small, rectangular chip roughly the size of a sim card. The blood flows through the top part of the device, while the bottom is lined with antibodies, which attach to any cancerous cells present in the sample. By looking inside the chip under a microscope, it is possible to determine if any cells have been captured and therefore if the blood sample contains cancerous cells.

An early problem with these devices was that the blood sample flowed too fast and too far above the antibodies, which meant that even when cancerous cells were present, they were not always detected. Later versions of the device shortened the distance between the top and bottom, but this meant that the blood sample had to be smaller, which in turn meant the results were less accurate. (The bigger the sample size, the more accurate the results.)
Karp wanted to know if there was a way to force the cancerous cells to slow down and better attach to the antibodies. So, instead of lining the bottom of the device with antibodies, Karp created synthetic jellyfish-like tentacles made out of DNA. The tentacles, which are roughly one-tenth the width of a human hair, are imbibed with a capturing agent that targets circulating tumour cells, and can extend to grab them. In tests of an early prototype, Karp found that his new design could increase the flow of blood by 10 times, making it far more likely that cancerous cells would be accurately detected.
We had moved downstairs to the aquariums cafe by the time Karp had finished laying all this out, and when I expressed some confusion about some of the details, Karp grabbed a napkin from a nearby table and retrieved a pen from his bag. It was in the shape of a bright orange crab claw. What? he said, in reference to my amused expression. I think its funny. I got it from a souvenir shop. He then proceeded to draw a diagram of his device on the napkin. (Karps business card features a very similar drawing of the tentacles, and a picture of jellyfish on the back, to show the process from inspiration to creation.)
Now, Karp said, leaning in conspiratorially. You want to touch a stingray?
In early 2011, Karp asked one of his graduate students, Maria Pereira, to help find a solution to the challenge that Pedro del Nido had set him: namely, how to seal holes in childrens hearts. We tried to define the key criteria for the problem: a material that couldnt be washed away by blood, was easy to deliver and minimally invasive, Pereira told me. Something that a surgeon could control.
Following Karps example, Pereira looked to the natural world for solutions. She held lab meetings and asked everyone to email her ideas or pictures of creatures that live in especially wet environments. People circulated photos of slugs and snails. We began thinking, how do snails stay attached to leaves when its raining? Karp told me. Why arent the trails they leave behind washed away by the rain? What are those secretions made of?
One day, someone emailed Karp and Pereira a link to a research paper on sandcastle worms, which live in shallow water on the Californian coast. The worms secrete a sticky, viscous goo that they use to build underwater shelters by gluing together bits of shells and sand grains. The goo is also hydrophobic meaning it repels water to ensure the shelter withstands the force of waves.
Slowly, Karp and Pereira began to imagine a product that would not only be used to treat small internal wounds in children, but that would have wider applications. They now envisioned a liquid surgical glue, strong enough to work in any major organ. It would be both biodegradable and capable of repelling blood and water.
In 2013, Karp co-founded Gecko Biomedical in Paris with the help of Bernard Gilly, the chairman of a group of small French biotech companies. Pereira later moved to Paris to join the company as its head of research.
Over the next few years, she and Karp tested different versions of the glue, each with a slight variation in viscosity or adhesive properties. Some versions were too runny and not sticky enough; other prototypes were so sticky they would not spread easily on to tissue. It was not enough to have the glue sit on top of the tissue it needed to infiltrate it, in order to create a perfect seal that would prevent air or blood from seeping through. Karp thought about how ivy attaches to the sides of buildings the plants root hairs seek out crevices and cracks, then secrete a glue that spreads the hairs in different directions. The hairs then shrivel up and dry in a spiral shape, which anchors the plant to its location. Many of the glue formulations did not work, but the ones that did worked very similarly to ivy, because they were able to burrow into the tissue, Karp said.
Karp and Pereira also developed a device in the shape of a pen, which emits a visible LED ray of light that reacts to the glue, so a surgeon can set the glue once it is applied. (The process takes five seconds.)
Each version of the glue was tested first in animal or human tissue inside the lab, and then inside a living organism, usually a rat or pig. The right version presented itself entirely by accident. Karp and Pereira set up an animal trial at Boston Childrens Hospital to test a new iteration of the glue: a small, circular patch rather than a liquid version. They created a hole inside the heart of a living rat, and were just about to seal it with the patch when it slipped off. They put it back on top of the hole, but by that point there was so much blood that the patch would not stay in place long enough for Karp to cure it with the light pen.
Scrambling for a solution, Karp asked Pereira to scrounge up as much of the most recent batch of liquid glue as she could. Pereira then spread the glue on to a spatula, and applied it to the leak in the rats heart. Karp followed with the light, and the glue set. It did exactly what it was supposed to it repelled the blood and it remained in place, Karp said. We ended up with a perfect seal. This was a massive hole, so showing that we can seal it without sutures or staples was a big deal to us. (When Karp and Pereira checked up on the same rat six months later, they found no signs of disability or stress. The glue on the animals heart had gradually biodegraded as tissue had grown over the patched up hole.)
Last spring, Karp showed off the glue during a talk at Zoobiquity, a semi-regular conference that brings physicians and veterinary surgeons together to swap notes. The event took place at the New England Aquarium, and Karp spoke from a semi-raised platform in front of the penguin pool. After the talk, a dental surgeon named William Rosenblad approached Karp to ask if he would be willing to give him some of the glue to use on one of his canine patients, a bulldog named Little Papi. Rosenblad had carried out three unsuccessful procedures to treat an oronasal fistula, a common problem in dogs and cats that results in a large hole in the mouth leading to the nasal cavity. He looked pretty desperate, Karp said. He just said, Get it to me as fast as you can.
A week later, Rosenblad sealed the hole in Little Papis mouth using Karps glue. I knew the real test would come when everything had healed, Rosenblad told me. Karp was present at the follow-up appointment two weeks later. Little Papi sat patiently while Rosenblad checked inside his mouth, finally declaring that the glue had worked the hole was sealed. We all got a bit emotional, Rosenblad told me. Little Papis owner walked up to Karp and shook his hand. He kept repeating, You changed my life, Karp said.
In March this year, after successfully raising 22.5m euros, Gecko began a trial of the surgical glue at four hospitals in Paris. The glue was tested on 36 patients, most of whom underwent vascular reconstruction surgery, in which blood vessels are either cut open to remove plaque or enlarged to enable better flow. Jean Marc Alsac, the surgeon overseeing the trial, said that it tested two things: one, how quickly the bleeding stopped when the glue was applied, and two, that there were no adverse effects in patients in the three months after surgery. It worked immediately, Alsac told me. I wasnt prepared for the surgery to be over that quickly. It was astonishing.
A human trial of the glue is planned for next year in the US. Karp hopes the glue will become part of the surgical armamentarium available in all hospitals throughout the world to reduce surgical times and complications of current procedures. He also wants to see it used in surgeries where there are currently no suitable methods to close tissues, such as in minimally invasive procedures where it is difficult to tie knots in small spaces, or where bulky stapling devices cannot fit. Currently, many surgical procedures are much more invasive than they need to be, he told me, but with better ways of sealing tissues in small spaces, this can drastically be reduced.
Making the glue indispensable to surgeons could also help boost bioinspirations profile, particularly in medicine. I think as others see successful examples, they will be more inclined to give it a try, Karp said. When I first started out, I didnt really see bioinspiration as a tool or platform merely a project. I certainly didnt realise how powerful it could be.
When I visited Geckos headquarters in Paris this summer, I asked Pereira to show me how the glue works. She filled a small syringe with 0.2ml of the glue, which is yellow and gloopy. She took a piece of clear rubber and pressed a small dot of glue on to its surface. Lets pretend this is a ruptured vessel inside the body, she said. She took a thin metal rod and spread the glue around on the rubber surface. She then took the pen light and held it over the rubber for five seconds. Here, she said, pushing the rubber into my hands. Feel it.
The glue had set into a shiny, flexible coating on top of the rubber. I played around with it for a few minutes, then asked Pereira if I could try applying the glue myself. She shook her head, laughing. Youll just have to wait your turn like everyone else.
This article was amended on 25 October 2016. An earlier version described Jeffrey Karp, who is an affiliate faculty member at MIT, as also running a lab at the university. His lab is actually affiliated with Brigham and Womens Hospital, where he is also a professor.
Follow the Long Read on Twitter at @gdnlongread, or sign up to the long read weekly email here